tv Frontline PBS November 13, 2012 10:30pm-11:30pm EST
10:30 pm
death is going to be my way. >> they can show you how to d. >> we lay out all of the options for them. >> and help you do it. >> take a good deep breath, and you will be asleep in no time. >> he wanted you all to think that he had died a natural death. >> a network of people commitd to a controversial idea. >> it was not about the right to die, end-of-life decisions. it was about the rule of law. >> she took her life, and they helped her do it. >> jana was not terminally ill; she just thought she was. >> inside the hidden world of assisted s.decisi >> today is thursday, and on sunday i am going to leave this earth. >> tonight ofrontline, "the suicide plan."
10:31 pm
>> frontlinis made possible by contributions to your pbs station from viewers like you. thank you. and by the corporation for public broadcasting. major support for frontline is provided by the john d. and catherine t. macarthur foundation, committed to building a more just, verdant and peaceful world. more information is available at macfound.org. additional funding is provided by the park foundation, dedicated to heightening public awareness of critical issues. and by the frontline journalism fund, with a grant from millicent bell, through the millicent and eugene bell foundation. major funding for "the suicide plan" is provided by the john and wauna harman foundation.
10:32 pm
(geese honking) >> it was a beautiful morning. the sun was out. and he said this was the day. he brought out this wretched rusty revolver. and i ran a cleaning rod through it to make sure that it was all right. he seemed a little uncertain as to just how to hold the weapon. if you tried to aim the weapon
10:33 pm
toward the top of your head, the trigger guard would interfere with your chin. so we concluded that if you turned it 90 degrees, that would be the way to do it. one of us suggested maybe he'd like to have a last smoke. so i got him his tobacco and his pipe, and he enjoyed that. and then he indicated that it was time. he took the gun-- he had loaded it-- and with the aid of his walker, we walked out to the garden. he chose the spot, and he decided he would lie down. so we said goodbye. and i shook his hand.
10:34 pm
i walked up the road a few hundred feet. i started to say, "god bless you," and i got "god bless" out when i heard the shot. he had put the revolver in his mouth, and it was instantly effective. and his pulse ceased soon after that. and i felt very sure that i could report that he was dead. >> narrator: john welles, a long-time friend of hunt williams, had been diagnosed with advanced prostate cancer a few months earlier. 66 years old and fiercely independent, john had always
10:35 pm
told friends that he would take his own life if he ever became incapacitated. >> to a man like john, this bear of a man who was reduced to an invalid, life didn't offer him anything after that. there are times, and certainly this was one of them, when one knows if what you did was right or not. and i had no question. that was probably why i explained it in such detail to the state police, because i felt that there's nothing to hide, and the more i explain, the more i cover exactly what happened, the better off we'll be. hindsight is 20/20. that wasn't the best move.
10:36 pm
>> narrator: hunt williams was arrested and charged with second-degree manslaughter for assisting in the suicide of john welles. if convicted, he would face up to ten years in prison. assisted suicide-- it's an age-old debate. the names are familiar. and so are the arguments, both pro and con. but it remains one of the most polarizing issues in america. two states-- oregon and washington-- have legalized doctor-assisted suicide, and only for the terminally ill. but around the country, people
10:37 pm
who want help dying aren't waiting for the laws to change. instead, they've gone underground. this is a journey told from the inside, far from public view. this is the hidden world of assisted suicide. >> i'm not afraid of dying. i've always believed that death is nothing to fear. it's part of living. everybody has to do it. and i want to make sure that my death is going to be my way. >> narrator: if joan foley butterstein lived in oregon or washington, an open conversation with a doctor could allow her to end her life the way she's always lived it, on her own terms.
10:38 pm
by age 18, joan had set out on her own. she was a singer and a dancer at the latin quarter in new york city. she married tom foley, her high school sweetheart, and began her life as a marine wife. nine years later, their daughter kathleen was born. life was good. but then, after 54 years of marriage, tom got sick. >> my husband died of lung cancer. and he went through chemo and radiation, and then more chemo and then more radiation. and he was sick and miserable frequently, if not most of that time. but because i saw how he suffered, i made up my mind,
10:39 pm
i... when it was my turn, i was going to make sure that i don't go that way. >> narrator: in 2006, joan got remarried to art butterstein, a 86-year-old widower. then, two years later, she found out that she too had lung cancer. >> i told them immediately. i said, "i have no intention of going through all the chemo. not at my age, and not with what i know is already wrong with my body. it's not going to make me have a lovely old life." all right, what about this? 34 down. >> "words seen in brackets." >> s-i-c, sic. >> a few months ago, she went to the doctor, and doctor said, "i think it might be time to sign up for hospice now." and that was the time that she actually got involved more so with compassion & choices. >> narrator: compassion & choices, one of the leading right-to-die organizations in america, has been spearheading the fight to legalize
10:40 pm
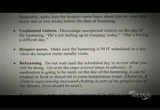
physician-assisted suicide, or what they call"aid in dying." but they also believe they can help people outside oregon and washington find ways to end their lives without breaking the law. >> it's our position that people who are terminally ill, who are looking at their death's approach not at some distant time in the future but "here it is, i'm approaching it now," those people can't and should not have to wait for absolute clarity on the law before they too are empowered with the means to control their suffering. >> seven principles for patient-centered end-of-life care. >> if a person is terminally ill and they come to compassion & choices for information, we lay out all of the options for them: stopping any medication or the therapy that is prolonging their
10:41 pm
life; discontinuing food and fluid and that would include stopping eating and drinking. and if none of those are available to them, we also talk with them about medication and we tell them what medications would be effective, we tell them a variety of ways that they could accumulate these medications, and we tell them that we will be with them at the bedside when they take medication that they know will cause a peaceful death. >> narrator: for terminally ill people like joan, who are enrolled in hospice, compassion & choices has developed "the protocol"-- a highly confidential document that gives step-by-step instructions about how to end a life using a lethal combination of medications. >> a few weeks ago, we got on the computer, with the counselor on the phone, and ordered her end-of-life medication, which kind of, for me, brought it home a lot. it's like, okay, now she can do this.
10:42 pm
>> it gave a whole list of different drugs that you wanted to order. and that i had already gotten from them exactly what milligrams i needed of this and this and this, and the purposes, the reasons for them. and i just checked off exactly what i needed, and it came in the mail. that was a big surprise. i couldn't imagine that this is available. but it is. >> she's got to take like 60 pills in like 15 minutes' time. she's got an anti-anxiety medication that she can take in case she's afraid at the time. and then there's an anti-nausea medication that she has to take, because the end-of-life medication that she takes, there's a lot of it, and it can upset your stomach.
10:43 pm
>> narrator: the protocol also warns families about the risk of discovery. empty medicine bottles should be removed, the protocol itself destroyed. and they're cautioned to tell as few people as possible. >> we have been well counseled by compassion & choices on who we can tell, and who we shouldn't tell. the hospice people can't know. the doctor can't know. it's just our little group, just, you know, the three of us and a couple of outside people who are there to support us after she's gone. after she's done it, i'm sure there won't be an autopsy or anything because she is terminal with lung cancer. so if she slips into a coma and dies, everyone will think it was just her cancer and the natural causes that did it.
10:44 pm
>> our perspective is what we do is absolutely legal, and we do not believe that we could be prosecuted or that there could be anything but a frivolous lawsuit brought against us. but nevertheless, the law is murky in the majority of the states. and so the organization draws its line. we have our eligibility criteria, we have our protocols, we have certain rules that we believe keep us on the right side of the law. we, under no circumstances, will ever be the source of the medication. we, under no circumstances, will absolutely ever be in the position of administering medication. no one does this to you. it is not euthanasia. it is not lying there and waiting for someone to administer the medication for you.
10:45 pm
>> narrator: although compassion & choices insists that what it does is legal, joan's counselor would not agree to go on camera, so the organization brght in another volunteer. >> we're here to talk about your request to be in charge of your dying. >> narrator: he is meeting with joan and her husband, art, for the first time to discuss what to expect if she takes the medication. >> this the lethal dose. typically, with this medication, you'd fall asleep in about a half hour, you'd go into a coma and 12 to 24 hours on average is when you would eventually die. >> i didn't realize that it would take that long, but i'm glad to know it. >> yeah, you know there is no magic pill. many people imagine that there's one pill that we provide and you
10:46 pm
just take it and you die, and there just isn't one. >> being present at someone's dying is heart wrenching. you become queasy, you become anxious. and it's not only from-from a person doing it, it's with any kind of death. looking back at my wife dying, it was... it's shattering. >> i don't want to be a burden. art's first wife, he took care of her for almost 12 years. she first started with heart problems and then she went into alzheimer's. and he took care of her but he was a lot younger then, too. >> i don't want her to go through the same physical situations that my wife did. i wouldn't want that, i wouldn't want that. i'm not... i'm catholic and i'm not in favor of this type...
10:47 pm
i wouldn't go through this myself. i wouldn't go through this compassion & choices business, but i can understand her feeling. for me, it would be a mortal sin to kill myself. but it has nothing to do with me. it all has to do with joan, her well-being, her feelings, and her desires. she knows what she wants. she's the only one that counts. >> when it comes down to the final ingesting of it, of drinking it, the compassion & choices counselor will say, "do you realize this can kill you and you still want to take it?" so even at the, right down to the last second there, your options are still available for you. >> compassion & choices has told us that i cannot help her. i will not feed her the medication. i will help her prepare it, but
10:48 pm
she will have to put the spoon to her mouth. she will have to put the pills down her throat. i'll give her the water to do it with, but she's going to have to take them. because that way, i can't... i-i can tell myself that i didn't kill her. that i didn't do it. she did it. she did what she wanted to do, in her own time, in her own way, but i didn't... i didn't give it to her. i didn't kill her. >> my counselor on the phone, she has found that almost 50% of her patients wind up not using their medications. and that may be me, i don't know, but i don't think so. >> i don't think any of us will be fully prepared. we'll make the effort, we'll steel ourselves to the point of no return, and we'll make sure that we go through it. and once it's complete, i'll
10:49 pm
hold her and i'll kiss her. >> none of us know yet what the day will be. it depends on how much longer i can stay as healthy as i am. i know i'm getting weaker. it's getting harder to get things done without help, without the oxygen. but i have what i need now, and good lord willing, i will be able to make that decision at the right time. i won't wait too long. if i can't get to the bathroom, and i can't go out anymore, and
10:50 pm
i'm locked in, and i'm just a burden, that's it. that's the amount of time i think god is giving me. and he's given me a wonderful life. >> we are split on many things in american society, and death is one of them that really is a pretty sharp dividing line. we're all conflicted as a society about these issues. so what happens is, it stays very underground and talking about it feels dangerous.
10:51 pm
if a person is ready to die, there are some legally acceptable ways that we can do out in the open. you take the example of taking somebody off a ventilator, which is a way, out in the open, in the hospital, we help people to die. we can do that and we document what we're doing. but when you start getting into an explicit assisting of somebody, when somebody really requests of you to hasten their death, that's a huge threshold to have to cross. and that's not going to happen very often.n >> narrator: dr. timothy quill made headlines in 1991 when he was brought before a new york state grand jury for prescribing a lethal dose of barbiturates to one of his terminally ill patients. >> it was not that different in my mind and in my personal experience from helping other
10:52 pm
people to die when i had taken them off a ventilator or helped them stop dialysis or done other things. these are big decisions. you only do them when you really have to do them. you do them when it's driven by a patient's suffering and their circumstance. so my experience of that psychologically and spiritually was not different. and i actually personally view them morally as not different. >> narrator: since going public with his case, dr. quill has become one of the leading advocates for legalizing physician-assisted suicide. >> one of the safeguards, in terms of legalization at least, is restricting it to people who have defined illnesses and who are terminally ill. that's a hard line for most people. certainly that would be a hard line for me if we're going to talk about assisted dying. but there are others in the movement who would say that it's the suffering that counts. when you get into the world of chronic illness, that's a much bigger world, much more complex
10:53 pm
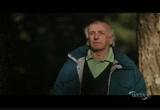
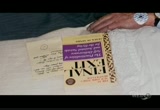
world. the further you go away from somebody who is dying anyway, in this domain of helping people to die, i think you're-you're getting on softer and softer ground. >> i've always argued that assisted medical dying should be for the terminally ill and the hopelessly ill. diseases like alzheimer's and als-- these terrible degenerative diseases. and they reach a point where they can go on no longer. >> narrator: derek humphry founded the first right-to-die organization in america and is considered by many to be the father of the movement. >> hello, my friends, i'm derek humphry. i founded the hemlock society in 1980 and, amongst other books, wrote that best-selling volume in 1991 called final exit.
10:54 pm
>> narrator: humphry's book, final exit, gives explicit instructions about the most effective ways to commit suicide, or what he calls "death by self-deliverance." a few years ago, he turned the book into a dvd. >> a light snack is necessary two to three hours before the time of the planned end. a full stomach slows down the effect of the drugs whilst a small amount helps absorption and reduces the chance of vomiting. it's a how-to, but it also goes into things like life insurance; family matters; suicide notes, yes or no; living wills. it's the hard facts of life and death. i must warn you that there are lots odrugs which will end life, but not pleasantly. they are risky in their deadliness and worse still have a terrible record of side effects.
10:55 pm
you can't just swallow a handful of drugs. you have to make preparations in your body, and in your timing. leave the copy of final exit at the bedside-- the mere presence of this book is a well-known indication to the authorities that this was a considered self-deliverance... millions of people want to know how to deal with their death when it's looming. they want to know that if they are trapped in a long, protracted illness, "what is my way out? perhaps this book gives me a way out." >> my father referred to the act of taking his life as "the plan." all members of our family, extended family included, knew of my father's intention to end his life.
10:56 pm
his neighborhood association knew of his intention to end his life. his close friends knew of his intention to end his life. that was well known. >> narrator: four years ago, george brodigan, an 82-year-old retired attorney from connecticut, had been diagnosed with dementia. although he'd been living on his own, he had recently started to decline and there was talk of him having to leave his home. >> he had seen friends suffer, whom he often talked about, and how wrong he thought it was that a rich and good life, and a fruitful life should end in such tragic, sad, helpless and anguished circumstances. and this is what he told people when he spoke of ending his life. he had an irreversible illness, and he was not going to go to an institution.
10:57 pm
it was simply, "i'll know when it's time to go." narrator: on september 14, 2010, george brodigan called his son bruce to tell him the day had come. >> when we arrived at his house, he had pretty much taken care of everything. he wrote out checks to loved ones. he put his obituary, which he wrote himself, and his life insurance policy on the dining room table, and he greeted us in a charcoal gray, pin-striped suit and a knit tie. once family members who wished to be with him that day but not be present at his death had had a chance to spend time with him and say goodbye, once they
10:58 pm
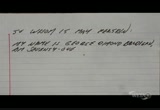
left, and there was just my dad and tom and me, there was sort of mutual acknowledgement-- it's time to go upstairs. and that's what we did. >> as we got into the bedroom, he was somber. he was quiet. but he was resolved. it seemed like he had thought hard and long, and-and he had come to this very difficult decision. and i think it's... it was almost as if he were tired and-and relieved to be... to be finally doing what he wanted to do. there was a bottle of rum on a bedside table, a glass, and a small tupperware container of pills. he also had on the... on the bed next to him the... a copy of the
10:59 pm
book final exit. >> i reminded him that he should write a note that this was his death, taken by his own hands, freely, and under no constraint. >> narrator: george wrote a number of drafts of his suicide note. in the final version, he got his age wrong, but it read, "there comes a time in all of our lives when it is time to say goodbye. this is where i am now at age 85." >> my dad sat up in the bed and proceeded to alternately take some pills with a teaspoon and with his hand, and drink some
11:00 pm
rum from... with ice. we waited for death to happen. all at a moment, he shut his eyes. he was still breathing regularly after that, for a time, and then he wasn't. i was advised, off the record, in conversations with lawyers and doctors, not to say that i had been present at my father's death, that i would seem
11:01 pm
heartless, callous, inhuman. and so i wrote up a short statement, and tom also wrote up a short statement, saying that we had not been present at my father's death. we simply went with the best advice we had, which was that it would be a gentle and sure death, and that if the police were called, it was none of their business what had been, to our way of thinking, a family affair, and only a family affair. >> narrator: but when police discovered that the pills george brodigan used to end his life were prescription medications that belonged to his son, bruce brodigan was arrested and he would spend the next year fighting manslaughter charges for assisting in the suicide of his father.
11:02 pm
>> it's almost impossible for the average citizen to obtain lethal doses of barbiturates. seconal and nembutal, the most quickly lethal, painless drugs in which to end life, are available only to doctors in oregon and washington for help to die. the authorities watch those drugs very carefully and doctors are very leery of dispensing them. myself and others realized that an alternative was needed. i brought together doctors from all over the world that i knew were interested in this. we had anesthesiologists and surgeons and nurses and lay people. after several meetings, we worked out that the best
11:03 pm
alternative method was the ingestion of helium gas. >> narrator: on june 20, 2008, sue celmer found her husband of 24 years, john celmer, dead in his home in cumming, georgia. ten days earlier john had undergone a complicated surgery, the latest in a two-year battle with cancer. >> i didn't know what happened. i had no idea what happened. did he take the wrong medicine? did he take too much medicine? did he... was he just... was his
11:04 pm
body just so weak that it couldn't withstand any more, and he lay down and just died? >> narrator: although the medical examiner ruled that john had died from natural causes, a week later, sue started to get suspicious. >> it wasn't right. there was something wrong. and until i started to go through his belongings that i inadvertently came across a couple of things that caught my attention. >> narrator: she discovered a number of items, including a copy of the book final exit, a receipt from party city for two helium tanks, and an email which john wrote on the day of his death. "i am most displeased with the results of the two surgeries and am considering 'my plan.' you know what i mean by that." >> john never said, "i am going to commit suicide."
11:05 pm
he never said, "i have a plan to end this." he, at times, would say, "i'm really tired of living like this." and that's natural. >> narrator: in 2006, john had been diagnosed with neck and throat cancer. although they were separated years earlier, the couple remained close, and at his wife's urging, he agreed to multiple surgeries and extensive radiation treatment, which left him cancer-free but physically disfigured and in chronic pain. >> there was a great deal of damage from the radiation and he began to lose teeth, and then his jaw bone actually severed on both sides. i know he was tired of living like that.
11:06 pm
but the prospects for him having a pretty full recovery were excellent. at no point ever was he told that he was terminal. ever. >> narrator: convinced that john never would have acted on his own, sue called the cumming police, who immediately asked the georgia bureau of investigations to get involved. >> whether mr. celmer wanted to end his own life and did it, the state didn't have an interest in that, as horrible as it is, as unfortunate as his death may be, suicide is not illegal, and that was certainly his choice. but with this case, we were talking about more than mr. celmer. >> narrator: the georgia agents discovered that a right-to-die group called final exit network
11:07 pm
had assisted in the suicide of john celmer. they also uncovered something called a "final exit log." it read: "left him in sleeping position; eyes were already closed. wife will discover next day." the log also indicated that a man named ted goodwin was somehow involved. >> my name is ted goodwin. i'm with final exit network. >> narrator: so the agents asked celmer's family to make an undercover call to ted goodwin to find out more about wt had happened. >> because of our conversations about suicide, he knew how i felt. it is not god's will that we
11:08 pm
take other people's lives or our own lives. that's very serious, even if you don't believe in god. there are laws in this country. who are you that you think that you have the ability or the right or the power to do that? >> narrator: goodwin also revealed that john had died by inhaling helium gas. ut >> i was not aware of this helium methodology that was used, and my first reaction is that if you want to talk about death with dignity, i don't think that it's going to involve helium tanks that are purchased from party city. it's creepy, it's disturbing. the concern grew that this was
11:09 pm
going on all over. this was an organized effort, if you will. literally it was an organization that was involved in it. >> narrator: final exit network was formed in 2004 when a faction of radical right-to-die activists broke off from compassion & choices. named after derek humphry's book, they also wanted to help non-terminal people like john celmer. and their president was ted goodwin. >> the network was designed to be supportive of anyone who was mentally competent and suffering more than they could bear. they did not have to be terminally ill. we feel this is an individual rights issue, that they should have the right to determine how they live and how they die. and we believe, at the heart of
11:10 pm
our mission, no person should die alone. >> narrator: members of final exit network meet once a year to review their policies and procedures. this year, they gathered at a hotel on the outskirts of chicago, and for the first time, they agreed to let cameras inside a network training session. >> this is a shortened version of our usual training. >> narrator: a largely volunteer organization, final exit network has over 3,000 members from all across the country. >> final exit network is a group of volunteers. we only half-jokingly refer to them as geriatric volunteers, because they are almost all old. they almost all seem to have had some experience themselves with coming very close to death. it has caused them all to think about it more than the average person. they see it as the next major civil rights issue, the civil
11:11 pm
rights issue of the 21st century. >> exit guide services are available to people who are members of our organization and meet our medical criteria. >> narrator: these volunteers call themselves "exit guides" and have been present at hundreds of planned deaths. >> i've been present at 41 exits. i have had exits in louisiana, texas, oklahoma, new mexico, arizona, colorado, utah, and even alaska. our method is an inhalation method. it's fast, it's painless and it's 100% effective. >> i look at death as being part of life, and that it's going to come to everybody, and that this person is very fortunate to be in a position of making a decision about how and when and under what circumstances it's
11:12 pm
going to happen for them. >> very, very few of the states have any definition of what it means to aid or assist. >> narrator: the exit guides are trained on what it means to assist and how to stay on the right side of the law. >> at the network, we believe that aiding or assisting requires either that you provided some implement, or that at the bedside you used your hands to do something active. under the network's protocols, you don't bring anything and you don't touch anything. never buy a helium tank, don't buy any parts. "don't touch anything" is the rule. >> narrator: the most critical part of the training centers on the network's recommended method of death. >> a death by helium is as peaceful a death as you will ever have. if someone put a hood over your head, carbon dioxide, carbon monoxide starts to build up, and your body senses air hunger, and it becomes very terrifying as it realizes that you're suffocating.
11:13 pm
helium is completely different than that. your body doesn't recognize the difference between oxygen and helium. you breathe four times, five times. it's very comfortable. it's just like you're breathing air. and then, boom, the lights go out. >> we'll show you what has been the usual equipment. >> narrator: the exit guides review all the equipment needed for what they call "the death event"-- a plastic hood, a tube, and a helium tank. >> the tubing should be, oh, about eight to ten inches inside when they place the hood on their head. helium is available in party stores or balloon stores and so on. and the hoods can be very easily made out of plastic bags that are at home. the earliest hoods that were
11:14 pm
used were turkey bags. >> so the patient can get the products they need without any problem at all. in other words, you don't need a physician to prescribe anything. it's totally in the patient's hands. >> two helium tanks have to be sort of removed before paramedics, police, firemen and all that. somebody, i guess, gets them into the car and drives to a dumpster somewhere. >> we think it's best that they are removed from the premises totally. >> narrator: but before any death event can occur, final exit network requires that all applicants be reviewed by its medical committee, formerly headed by dr. lawrence egbert, a retired anesthesiologist. >> all the patients are asked to send their medical records in and we have a letter from the patient about why i want to die in writing so i'd have all that available. i would then evaluate that and then i would say, well that's easy, that's straightforward,
11:15 pm
the patient has a horrible pain, the patient has a horrible loss of dignity and therefore i would write accepted. in the time that i was medical director for final exit network, i approved approximately 300 cases and probably rejected ten. >> i think the majority of patients are quite content with helium. one reason that some don't is the idea of having this balloon over the top of your head. the balloon has the lack of dignity, but so does taking sleeping pills. it has nowhere near the loss of dignity that a shotgun carries, or a rope. let's see, i've got a bag here. >> narrator: dr. egbert insists that anyone who uses the helium method is completely in control, and makes the final decision alone. >> the point of no return is when a patient pulls it down and that's made very clear to them. and i often will say, "once you pull it down, you've made the decision.
11:16 pm
if you pull... full of helium, pull this down over your head, you'll be unconscious between 30 and 60 seconds, and unless you have a very vigorous, strong heart, dead within eight to ten minutes. when a person dies, then we'll take the bag off. and after they... we've sat for a few minutes. that way, if the relatives are there, we'll ask them explicitly to wait a couple of hours, so the body will cool, so that somebody won't try and resuscitate. if they try and resuscitate right away, they can get a heart... the heart's very tough and the brain is not so tough. so the heart will start up again. and i've seen a person like that where the heart started up beautifully, normally, but the brain was totally dead. and that, we do... that is the ultimate of disasters. >> i mean, the secret world is hugely problematic, because the
11:17 pm
edges are not clear. there's only a certain amount of rigor you can bring to this if you're coming in as a stranger into a person's life. you don't know them beforehand. the stakes are really high, and you want to be as sure as you can be. you have to have some medical sophistication, some experience dealing with suffering and the kind of nuances of that. what happens in the underground system is that process of evaluation gets truncated if it occurs at all. so you don't have this opportunity to try to relieve the suffering by somebody who understands suffering. you have a lot of very well- meaning, compassionate people who are doing this out of the good of their heart. but i think it's very... it's very tricky and dangerous in a certain way.
11:18 pm
>> narrator: on february 13, 2007, 58-year old jana van voorhis of phoenix, arizona, applied to final exit network for help. two months later, she was found dead in her home. >> tom and i got a call from somebody saying they were from jana's church. "you know how she's always sick," she said to me, "and i think you should go check on her." so we decided we better go over to her house and see if she was okay. >> it was mid-afternoon, mid to late afternoon. i went in and found jana dead in bed. >> i said, "i want to go in," and he said, "i don't know if you want to see her," and i said, "i have to." and so he took me back to her bedroom, and there she was. and she was dead, and she had blood coming from her mouth.
11:19 pm
>> the initial medical report called it a natural death, probably by some kind of heart in it wasn't till later, when we started digging into things more deeply, going through messages on jana's answering machine, looking at things, and i think finally finding the final exit network brochure, that things started to click. and that's when we started calling the police department and said, "we think something's kind of screwy here." >> the thomases received a telephone call, and the caller stated she was a friend of jana's, she was from jana's church. "can you please go and check on her?" well, they have caller id. viki and tom thomas have caller id. and on that caller id was the name frank langsner. >> narrator: so phoenix homicide detectives lois weiss and her partner jennifer mellinger drove out to meet with frank langsner.
11:20 pm
>> narrator: they recorded the meeting. >> narrator: at first, langsner denied being involved in jana's death, but then the detectives told him about the phone call with his caller id. >> once we started talking to mr. langsner, he just started providing us more information as far as what his involvement was. he mentioned wye hale-rowe being involved as the senior exit guide, who basically was, for lack of a better word, his mentor. >> narrator: langsner also
11:21 pm
described to the detectives all the reasons jana wanted to die. >> i think i was the first person that met jana personally. as i recall, i think she had gotten the tanks right away, within a week. and so that was an indication to me that she's ready to do it. she was a little anxious. she was concerned, will she gag or will she choke? wye assured her that she had a lot of experience and was going
11:22 pm
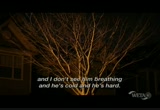
to help her through this, and it would be an easy kind of a thing for her. >> she was a lady who was tired of hurting, she was tired of being upset, she was just tired of living. "i just don't want to live anymore." we went back to it several times, and it was just the same themes. "i just don't want to live." >> the night of the death event, jana knew that she had to do everything herself. she had to go get the tanks, which she had stored in her house. she had to hook up the tubes. she had to adjust the hood. all of that went smoothly, and she was ready to go. >> we set her up and told her
11:23 pm
how to arrange herself in bed, and went on with the procedure. after we reached the point where the hood was filled with helium, she had turned on the valves, i talked to her about, did she understand what she was asking? and when you... "you will never wake up. do you understand that?" and she just thought it was absurd. of course she wasn't going to wake up. she wanted to die. >> i was at the foot of the bed, watching. and she smiled at me and kind of gave me a nod as if to say, "i'm okay." >> i had my hand on her wrist, on her pulse on one hand, and
11:24 pm
was just simply holding the other one. most people want some contact while they're leaving. and she had a lot of anxiety, and she wanted to hold on. >> wye told her, "take a good deep breath and you will be asleep in no time, in 30 seconds or 40 seconds." and she was looking at me and looking at wye, and that was it. >> and we put her in a sleeping position and we left the house. took all the apparatus with us. i felt that the death had gone well, and that we had done what we wanted to do. but this was against the background. i assumed that she was
11:25 pm
critically ill. >> jana was not terminally ill. she just thought she was. she was convinced she had breast cancer, liver lesions, blood disorders, many things that doctors did test and test and test and found nothing. it was very apparent that she was mentally ill. she, in the last couple years, had been in psychiatric hospitals. the psychiatrists described jana's psychiatric problems as hypochondriac and delusional and psychotic and schizophrenic. >> narrator: jana had been battling mental illness since childhood. she had been hospitalized multiple times.
11:26 pm
her psychiatric records, spanning more than 40 years, suggest a lifetime of suffering. >> over the years, jana would get progressively worse. and then she'd be committed again and seem a little better for a little while. and it was just a pattern that was followed. >> she certainly had disordered communication, and it took some work to help her complete the sentences, but she certainly had thinking behind it. sometimes an illness itself has some cognitive components, and people have difficulty communicating. and so my concern about her cognition was, does she understand the consequences of what she is requesting?
11:27 pm
does she understand finality? does she know what's going to happen? and she explicitly knew. but it was deeply disappointing to find out, for me, that none of those physical diagnoses, medical diagnoses, were real, and that this had not been validated by the medical committee of final exit network. >> the man that's supposed to be the medical director of this final exit network organization received actually nothing from any medical personnel, nothing from a hospital, nothing from a doctor. he received a little handwritten thing about her exposure to rat poisoning, bugs eating her, and some of the illnesses she did have over the previous 20,
11:28 pm
25, 30 years. now, how this so-called medical director didn't say, "something is really wrong here. let's step back, let's take a look at this lady and see what's really wrong with her." how that happened is... i don't know. i don't know. >> we accept, at least theoretically, any individual patient with a disease that's causing unacceptable suffering by their definition, not by our definition, and that, of course, would include mental diseases. jana van voorhis, it was so clear what her problems were. it was also very clear, even on paper, that she'd done a lot of suffering for a lot of years. i was told she wanted to die and then evaluated the case, thought it was acceptable, wrote "accepted," and then told the coordinator that she was accepted medically, and that's all i did.
11:29 pm
>> narrator: the death of jana van voorhis soon turned into something much larger than a single assisted suicide case. >> our investigation involving jana van voorhis was multi-state. jennifer and i were approached in the summer of 2008 by the georgia bureau of investigation, looking for some assistance in one of their cases. and it did spider web. it almost felt like somebody hitting a rock against a windshield and it just fractures. it was multi-jurisdictional, multi-agency, also multiple suspects. we're not dealing with just one person. we wanted to have the long arm of the law reach out and grab other persons in other states. so we decided to go after this. and we decided to go after the organization of the final exit network. >> narrator: with the hope of taking down the entire organization, the detectives joined forces with the georgia auit
306 Views
IN COLLECTIONS
WETA (PBS) Television Archive
Television Archive  Television Archive News Search Service
Television Archive News Search Service 
Uploaded by TV Archive on

 Live Music Archive
Live Music Archive Librivox Free Audio
Librivox Free Audio Metropolitan Museum
Metropolitan Museum Cleveland Museum of Art
Cleveland Museum of Art Internet Arcade
Internet Arcade Console Living Room
Console Living Room Books to Borrow
Books to Borrow Open Library
Open Library TV News
TV News Understanding 9/11
Understanding 9/11